Abstract
With the adoption of reduced-intensity conditioning (RIC) regimen, allogeneic hematopoietic cell transplantation (alloHCT) is being increasingly used in older adults. However, data are sparse on the safety and efficacy of this procedure in patients aged ≥70 years. Currently the majority of these patients receive either non-myeloablative busulfan (Bu; 3.2-6.4mg/kg) or low-dose total body irradiation (TBI; 2-4.5Gy)- based conditioning regimens, which are associated with a relatively high incidence of disease relapse.
We report here the transplant outcomes of patients aged ≥70 years with hematological malignancies who underwent alloHCT with melphalan (Mel)-based conditioning regimen (Mel 100-140mg/m2 plus fludarabine or clofarabine) between May 2007 and September 2016 at City of Hope. We evaluated 53 consecutive patients (median: 71, range: 70-78 years, 35 males and18 females) who underwent AlloHCT for acute myeloid leukemia (n=27), myelodysplastic syndrome (n=14), myeloproliferative neoplasm (n=6), acute lymphoblastic leukemia (n=2), non-Hodgkin lymphoma (n=2), blastic plasmacytoid dendritic cell neoplasm (n=1), or acute promyelocytic leukemia (n=1) from HLA-identical sibling (n=11), matched unrelated donor (8/8, n=38) or mismatched unrelated donor (n=4). Fifty-one patients received peripheral blood stem cell grafts while two received bone marrow grafts. Graft versus host disease (GVHD) prophylaxis was tacrolimus/sirolimus-based in all patients. The disease risk index (DRI) score was high-very high in 36% of patient (n=19) and Karnofsky score was ≥70% in all patients. The HCT comorbidity index was 3 or more in 21 patients.
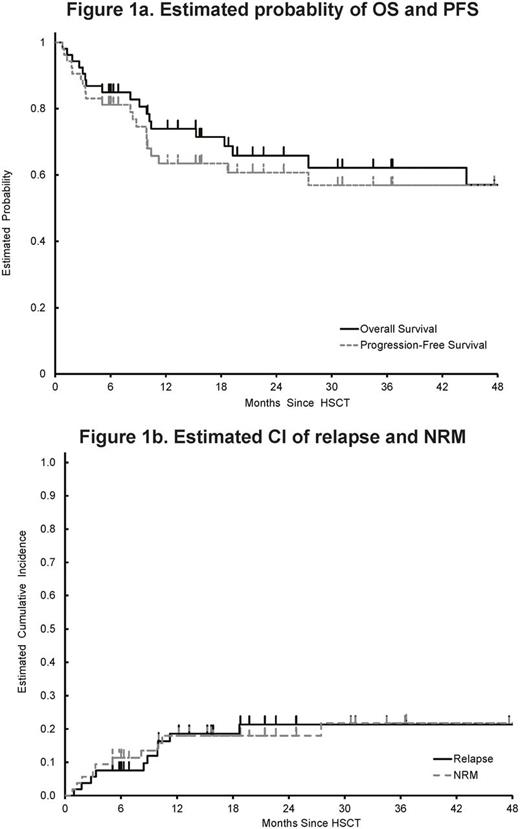
Fifty-two of our 53 patients achieved neutrophil engraftment with the median time to engraft of 15 days (range: 11-29 days). Blood or bone marrow chimerism analyses showed >95% of patients achieved >95% donor chimerism within 6 weeks from alloHCT, consistent with "semi-ablative" nature of Mel-based RIC. With a median follow up of 22 months (range: 5-99 months), the 2-year overall survival (OS) and progression-free survival (PFS) were 65.8% (95%CI: 49.9-77.7%) and 60.7% (95%CI: 45.2-73.0%), respectively (Figure 1a). Cumulative Incidence (CI) of non-relapse mortality (NRM) at 1 and 2 years were 18% and 18%, and CI of relapse at 1- and 2-years were18.6% and 21.3%, respectively (Figure 1b). 100-day CI of grade II-IV acute GVHD was 37.7% (grade III-IV: 18.9%), and 2-year CI of chronic GVHD was 57% (48% extensive). In multivariate high/very high DRI was the only independent predictor for poor OS was (HR: 3.14, 95%CI: 1.29-7.61, p=0.011).
While clinical outcomes were favorable for the most part, the hospital course was complicated by ICU transfer (24.5%, n=13) and altered mental status or fall requiring CT scan of the brain (24.5%, n=13), with the median duration of hospitalization of 33 days (range: 20-147 days). Blood stream infection (BSI) was developed in 11 patients (21%). Only 2 patients (3.8%) developed probable/proven invasive fungal infection (one patient developed Aspergillus fumigatus and the other patient developed Cryptococcus gatti). While CMV viremia was observed in 13 patients (24.5%) no CMV disease was diagnosed in any of these patients. Of the 49 discharged patients, 48 went home (one to rehab facility).
In conclusion, alloHCT in combination with Mel-based semi-ablative conditioning is associated with acceptable toxicities including NRM, low-risk of relapse, favorable OS and relapse free survival (RFS) in patients ages 70 years and older. Our data collectively suggest that chronological age alone should not exclude patients from undergoing alloHCT, and this treatment should be offered to selected older individuals with hematologic malignancies.
Nademanee: seattle Genetics: Speakers Bureau. Stein: Stemline: Consultancy; Amgen: Consultancy, Speakers Bureau.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal